Imagine a world where the fight against life-threatening diseases transcends established boundaries. Picture a future where innovative solutions challenge the conventional methods in combating one of the most formidable ailments of our time. The quest to discover an optimal cure, which can revolutionize the way we treat diseases, has become an emblematic pursuit for scientists and healthcare professionals worldwide.
Within this realm of relentless dedication to human wellbeing, lies the ambition to unlock the secrets to an efficacious remedy that can alleviate the burden imposed by the afflictions that haunt us. It is a fervent and ceaseless journey that aims to revolutionize the narrative surrounding the eradication of ailments, ushering in a paradigm shift that will unequivocally alter the course of medical history.
Underneath the surface of this ardent pursuit lies an amalgamation of ingenuity, perseverance, and hope. Experts from diverse fields, including oncologists, geneticists, pharmacologists, and beyond, unite in their desire to curtail the suffering brought about by malignancies. Their unwavering commitment is underpinned by an unwritten pact that envisions a future liberated from the shackles of devastating diseases, and envisions a tomorrow brightened by the possibilities that groundbreaking therapies can bring.
Unleashing the Power of Immunotherapy: A Promising Approach in the Fight Against Cancer

Imagine a future where the body's own immune system becomes the leading weapon in the battle against cancer. In recent years, there has been a growing interest in harnessing the potential of immunotherapy, a revolutionary approach that seeks to activate and enhance the body's natural defense mechanisms to target and destroy cancer cells. Unlike traditional treatments such as surgery, chemotherapy, and radiation therapy, immunotherapy aims to stimulate the immune system and unleash its inherent power to recognize and eliminate cancer cells, offering a promising avenue for the development of highly targeted and effective cancer treatments.
At its core, immunotherapy works by leveraging various components of the immune system, including T cells, B cells, and natural killer cells, to recognize and attack cancer cells. This approach takes advantage of the immune system's ability to distinguish between healthy cells and abnormal ones, thereby avoiding the often debilitating side effects associated with conventional treatments. By bolstering the immune response, immunotherapy holds the potential to not only eradicate existing tumors but also provide long-term protection against cancer recurrence.
- Checkpoint inhibitors: These drugs target specific proteins on cancer cells or immune cells, blocking the mechanisms that inhibit the immune response. By removing these checkpoints, the immune system is unleashed and can mount a robust attack on cancer cells.
- Adoptive cell transfer: This revolutionary technique involves genetically modifying a patient's own T cells to express specific receptors that recognize cancer cells. Once reintroduced into the body, these engineered T cells effectively seek and destroy cancer cells.
- Cancer vaccines: Acting as a form of preventive medicine, cancer vaccines aim to train the immune system to recognize and target cancer cells. These vaccines can be tailored to individual patients, offering a personalized and targeted approach.
While immunotherapy has shown significant promise in the treatment of certain cancers, more research is needed to optimize its effectiveness and expand its applications to a wider range of cancer types. Challenges such as resistance to immunotherapy and understanding the complex interactions between cancer cells and the immune system need to be addressed. However, with ongoing advancements and breakthroughs in this field, we can envision a future where immunotherapy plays a pivotal role in transforming cancer treatment, offering new hope and brighter prospects for patients worldwide.
Revolutionizing Cancer Treatment: The Potential of Targeted Therapies
Envisioning a transformation in the way we combat the formidable disease looming over countless lives globally, innovative solutions have emerged to redefine the course of cancer treatment. Unlocking the potential to revolutionize conventional approaches, targeted therapies hold significant promise in the fight against cancer.
By honing in on specific molecular alterations or characteristics unique to cancer cells, targeted therapies aim to disrupt the cellular processes driving cancer growth and proliferation. Unlike traditional treatments, which often affect both healthy and cancerous cells, these therapies strive to selectively attack cancer cells, minimizing the detrimental impact on the patient's overall well-being.
- Personalized Precision: Targeted therapies take into account the distinct genetic and phenotypic variations exhibited by different tumors, enabling a personalized treatment approach tailored to individual patients. By identifying and targeting specific alterations present in cancer cells, these therapies increase the likelihood of successful outcomes while minimizing treatment-related toxicity.
- Providing Alternatives: For patients who may not be suitable candidates for conventional treatments such as chemotherapy or radiation therapy due to factors such as age or health status, targeted therapies offer a ray of hope. The ability to target specific vulnerabilities unique to cancer cells opens up new pathways for effective treatment, especially for those deemed unfit for traditional modalities.
- Reducing Resistance: One of the major challenges in cancer treatment is the development of resistance to conventional therapies over time. Targeted therapies, however, hold the potential to address this issue by targeting specific signaling pathways or genetic alterations that drive resistance mechanisms in cancer cells, hindering their ability to evolve and adapt.
- Combination Approaches: Targeted therapies can also be used in combination with other treatment modalities to enhance their effectiveness. By synergistically targeting multiple aspects of cancer growth and survival, these combination approaches hold great promise in overcoming drug resistance and achieving improved outcomes.
- Pioneering Research: The development and refinement of targeted therapies rely heavily on ongoing advancements in the field of molecular biology and genomics. By unraveling the complex molecular underpinnings of cancer, researchers are paving the way for the discovery of novel targets and the development of innovative therapies that continue to push the boundaries of cancer treatment.
As we embark on this transformative journey towards a future where cancer can be effectively managed and defeated, the potential of targeted therapies shines as a beacon of hope. By capitalizing on the unique characteristics of cancer cells, these therapies offer a promising avenue to revolutionize cancer treatment, delivering renewed optimism to patients and healthcare professionals alike.
Integrative Medicine: Exploring the Role of Complementary Treatments in Oncology

As medical advancements continue to push the boundaries of cancer care, the integration of complementary treatments into traditional therapies is gaining recognition. This section aims to delve into the emerging field of integrative medicine in oncology, focusing on the role of complementary treatments in supplementing conventional cancer treatments.
Integrative medicine embraces a holistic approach to patient care, combining evidence-based conventional medicine with complementary therapies such as acupuncture, herbal medicine, mindfulness, and nutrition. By incorporating these complementary treatments, healthcare professionals aim to enhance the overall well-being and quality of life for cancer patients, reducing side effects and optimizing treatment outcomes.
A critical aspect of integrative medicine is its emphasis on personalized care. Recognizing that not all cancer patients are the same, healthcare providers tailor treatment plans by considering a patient's unique medical history, symptoms, lifestyle, and preferences. This individualized approach allows for a comprehensive assessment of potential complementary therapies that may be most beneficial for each patient, ultimately promoting better patient outcomes and satisfaction.
Complementary treatments can address a range of cancer-related challenges, including pain management, nausea, fatigue, and psychological distress. For instance, acupuncture has shown promising results in alleviating chemotherapy-induced nausea and vomiting, while mind-body practices like meditation and yoga have been effective in reducing anxiety and improving overall mental well-being.
| Complementary Treatment | Specific Benefits |
|---|---|
| Acupuncture | Relief of chemotherapy-induced nausea and vomiting |
| Mindfulness and Meditation | Reduced anxiety and improved mental well-being |
| Herbal Medicine | Potential antioxidant and anti-inflammatory effects |
| Nutrition | Supporting immune function and optimizing overall health |
However, it is crucial to acknowledge that complementary treatments should never replace conventional cancer treatments. Instead, they should be integrated into a comprehensive care plan under the guidance of healthcare professionals. Collaborative efforts between oncologists, complementary therapists, and patients are vital to ensure the safe and effective implementation of complementary treatments.
As the field of integrative medicine continues to evolve, ongoing research is essential to expand our understanding of the benefits and limitations of different complementary therapies. By combining the best of conventional and complementary medicine, we can strive for a multidimensional approach towards cancer care, offering patients a brighter and more comprehensive future.
Advancing the Battle Against Cancer: Embracing the Promising Landscape of Precision Medicine
In the ever-evolving quest to conquer one of humanity's most prolific adversaries, cancer, scientists and researchers alike are entering an era where precision medicine holds tremendous potential. This emerging field, which aims to tailor treatment strategies based on an individual's unique genetic makeup and other specialized factors, is set to revolutionize the way we combat this complex disease. By harnessing the power of advanced technologies and personalized therapies, precision medicine offers a beacon of hope in our collective mission to eradicate cancer and pave the way for a brighter future.
- Unleashing the Power of Genomics: Unlocking the Mysteries Within
- Targeting Tumor Mutations: Aiming for Bullseye Accuracy
- Immunotherapy: Harnessing the Body's Defense System
- Emerging Biomarkers: Illuminating New Paths for Diagnosis and Treatment
- Understanding Epigenetic Changes: Rewriting Cancer's Genetic Script
- Novel Drug Delivery Systems: Enhancing Efficacy and Reducing Side Effects
- Precision Imaging: Enabling Early Detection and Enhanced Treatment Monitoring
- The Role of Artificial Intelligence: Enhancing Cancer Diagnosis and Treatment Decision-Making
As precision medicine continues to gain momentum, it is becoming increasingly clear that the future of cancer treatment lies in customization and individualization. By delving into the intricacies of a patient's genetic profile, lifestyle choices, and environmental factors, healthcare professionals can tailor interventions that maximize effectiveness and minimize potential adverse effects. This approach promises to transform cancer care from the current one-size-fits-all model to a tailored, precise, and patient-centric paradigm.
Although challenges and hurdles remain, the strides made in precision medicine exemplify the dedication and determination of the scientific community to transcend traditional boundaries and strive for breakthroughs in cancer treatment. By embracing this innovative approach, we breathe life into the dreams of a society free from the burden of cancer, bolstering collective hopes for a brighter, healthier future.
Hope on the Horizon: Breakthrough Advances in Cancer Research

In this section, we will explore the promising developments in the field of medical science that are bringing us closer to overcoming one of the most formidable challenges humanity faces today. Cutting-edge research and groundbreaking discoveries are ushering in a new era of hope for individuals affected by this pervasive and complex disease.
The relentless efforts of scientists, doctors, and researchers have paved the way for remarkable breakthroughs in the understanding, prevention, diagnosis, and treatment of cancer. These advancements are providing renewed optimism and a sense of possibility for patients and their loved ones worldwide.
Some of the exciting progress includes innovative approaches to targeted therapies, with precise treatments designed to attack cancer cells while minimizing damage to healthy tissues. Remarkable advancements in immunotherapy have also emerged, harnessing the power of the body's immune system to detect and destroy cancer cells. In addition, personalized medicine strategies are being developed to tailor treatments to an individual's unique genetic profile, maximizing effectiveness and minimizing side effects.
Furthermore, groundbreaking discoveries in cancer genetics, genomics, and epigenetics have shed light on the underlying mechanisms of the disease, providing valuable insights into its development and progression. This knowledge is fueling the development of novel therapeutics and preventive strategies, offering newfound hope and potential for a future where cancer is no longer a devastating diagnosis.
It is important to acknowledge that while these advancements hold great promise, there is still much work to be done. Clinical trials, rigorous testing, and ongoing research are essential to translate these breakthroughs into tangible treatments that can be accessible to all who need them.
As we continue to push the boundaries of scientific knowledge and collaborate across disciplines, the dream of a world without cancer is edging closer to reality. The tireless dedication of medical professionals, the indomitable spirit of patients, and the support of society as a whole are invaluable in driving the quest for a brighter future, where cancer no longer holds the power it once did.
Beyond Chemotherapy: Innovative Drug Delivery Systems for Enhanced Cancer Therapies
In the quest to revolutionize cancer treatment strategies, scientists and researchers are actively exploring novel drug delivery systems that go beyond traditional chemotherapy approaches. By seeking innovative ways to administer anticancer drugs, experts aim to optimize therapeutic outcomes and minimize adverse effects, ultimately leading to a brighter future in cancer care.
As the understanding of cancer biology deepens, it becomes apparent that a one-size-fits-all approach to treatment is not sufficient. Different tumors exhibit unique characteristics and respond variably to conventional therapies. It is in this realm that the development of tailored drug delivery systems gains significance, offering the potential for personalized and more effective approaches to cancer treatment.
One promising area of research involves nanotechnology-based drug delivery systems. Utilizing nanoparticles, liposomes, or micelles as carriers, researchers can enhance drug solubility, stability, and bioavailability, leading to improved anticancer drug delivery. These smaller-sized carriers can penetrate and accumulate within tumors by exploiting the enhanced permeability and retention effect, maximizing drug concentration at the desired site and minimizing off-target effects.
Another avenue being explored is targeted drug delivery, utilizing ligand-receptor interactions specific to cancer cells. By conjugating anticancer drugs with ligands that recognize overexpressed receptors on tumor cells, researchers can increase selectivity and reduce toxicity to healthy cells. This targeted approach holds great promise in improving treatment efficacy, as it allows for higher drug concentrations within tumor cells while sparing normal tissues.
Furthermore, emerging technologies such as transdermal patches, implantable devices, and injectable hydrogels offer alternative routes for delivering anticancer drugs. These innovative delivery systems provide controlled and sustained release of therapeutic agents, enabling continuous treatment and reducing the dosing frequency. Additionally, they can bypass gastrointestinal degradation, ensuring higher drug bioavailability and minimizing systemic toxicity.
In conclusion, the pursuit of enhanced cancer treatments extends beyond traditional chemotherapy options. By harnessing the potential of innovative drug delivery systems, scientists aim to overcome the limitations of current therapies and strive towards a future where personalized, targeted, and minimally toxic treatments provide hope for patients worldwide.
The Role of Genetic Testing in Tailored Cancer Therapy
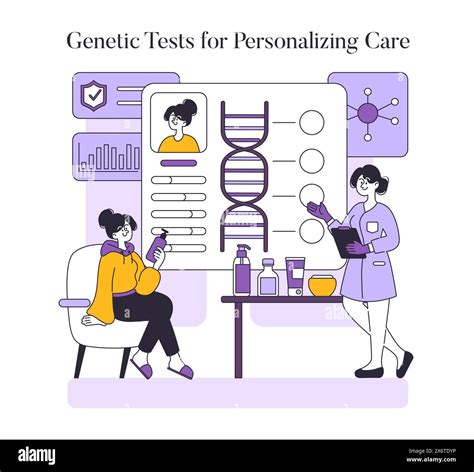
In the quest for personalized approaches to cancer treatment, the role of genetic testing has emerged as a crucial factor in determining tailored therapies for patients. By analyzing an individual's genetic makeup, this diagnostic tool provides valuable insights into the unique molecular profile of a tumor, enabling healthcare professionals to identify specific genetic mutations or alterations that drive cancer growth. Such information paves the way for precision medicine, where treatment plans can be customized to target the specific genetic abnormalities present in each patient.
Unveiling Genetic Anomalies
Genetic testing allows for the identification of specific genetic anomalies within an individual's DNA, providing a deeper understanding of the underlying causes behind the development and progression of cancer. By detecting mutations in certain genes, such as BRCA1 and BRCA2, which are associated with an increased risk of developing breast and ovarian cancer, healthcare providers can guide patients towards appropriate preventive measures or treatment strategies. These tests can also identify specific genetic alterations that make tumors susceptible to certain drugs, assisting in drug selection and maximizing treatment efficacy.
Personalizing Treatment Strategies
The information obtained from genetic testing plays a pivotal role in personalizing treatment strategies for cancer patients. By identifying the specific genetic abnormalities driving cancer growth, healthcare professionals can design individualized therapies that target these specific alterations. This approach can lead to improved treatment outcomes and reduced side effects, as therapies can be tailored to address the unique characteristics of each patient's cancer. Furthermore, continuously monitoring genetic changes through testing allows for adjustments in treatment regimens, ensuring that therapy remains effective as cancer cells evolve.
Challenges and Future Directions
While genetic testing presents immense potential in advancing personalized cancer treatment, certain challenges and considerations need to be addressed. These include the accessibility and affordability of testing technologies, the interpretation and management of complex genetic data, and the need for proper informed consent and counseling for patients. Additionally, ongoing research and technological advancements are essential to refine and expand our understanding of the genetic basis of cancer, enabling the development of more targeted therapies and further improving patient outcomes.
In conclusion, genetic testing plays a critical role in tailoring cancer therapy by revealing genetic anomalies, guiding treatment selection, and individualizing treatment strategies. Despite challenges, the integration of genetic testing into routine clinical practice holds promising prospects for enhancing personalized cancer treatment and bringing us closer to a future where effective therapies are available for all.
Enhancing Survivorship: The Significance of Supportive Care in the Management of Cancer
Surviving cancer and achieving positive outcomes require more than just effective medical treatments. Supportive care, an integral component of cancer management, plays a crucial role in enhancing the overall well-being of cancer patients. By addressing their physical, emotional, and psychosocial needs, supportive care helps patients cope with and overcome the challenges associated with cancer and its treatment.
- Enhancing Quality of Life: Supportive care focuses on improving the quality of life for cancer survivors by managing the symptoms and side effects of the disease and its treatment. This includes providing pain management, nausea relief, and assistance with maintaining activities of daily living.
- Promoting Emotional Well-being: Cancer treatment can often lead to emotional distress, such as anxiety and depression. Supportive care offers psychological support and counseling services to help patients navigate and cope with the emotional challenges that arise during and after cancer treatment.
- Addressing Practical Concerns: Survivors may face various practical challenges, including financial burdens, employment difficulties, and insurance issues. Supportive care provides assistance in navigating these concerns, offering guidance on resources and support programs available to ease the burden.
- Supporting Rehabilitation and Survivorship: Cancer treatment can leave survivors with physical impairments or limitations. Supportive care includes rehabilitation programs aimed at restoring physical function and promoting overall well-being. Additionally, survivorship programs provide guidance for transitioning back to normal life and maintaining long-term health.
- Empowering Patients and Their Families: Supportive care actively involves patients and their families in decision-making and encourages open communication with healthcare providers. This involvement empowers patients and their families to actively participate in their care, fostering a sense of control and ownership over their journey.
In conclusion, the provision of supportive care is essential in the holistic care of cancer patients, going beyond medical treatments to address the diverse needs and challenges they face. By enhancing survivorship through symptom management, emotional support, practical assistance, rehabilitation, and patient empowerment, supportive care holds immense value in promoting positive outcomes for cancer survivors.
Ethical Considerations in Oncology: Harmonizing Expectations, Quality of Life, and Financial Burden

When contemplating the intricacies of cancer treatment, it is crucial to navigate the ethical implications that arise from the delicate balance between hope, quality of life, and cost. As medical advancements continue to fuel our dreams of a future free from the perils of cancer, it is imperative to address the ethical considerations that accompany the pursuit of effective treatment options.
Striking a Balance Between Hope and Realism
Patients facing a cancer diagnosis are undoubtedly fueled by hope, seeking effective treatments that promise a brighter future. However, it is crucial to strike a delicate balance between providing realistic expectations and fostering a sense of optimism. Healthcare professionals must navigate the ethical landscape by ensuring patients are well-informed about the potential benefits and risks of different treatment options, while managing expectations to avoid false hopes and undue suffering.
Enhancing Quality of Life Alongside Treatment
Cancer treatments often come with physical and emotional burdens that impact a patient's quality of life. Ethical considerations arise when determining the best course of action to alleviate symptoms and improve overall well-being. Palliative care, for instance, focuses on addressing pain and discomfort, providing emotional support, and enhancing the patient's quality of life. By incorporating palliative care alongside standard treatment protocols, patients can experience a more holistic approach that emphasizes their well-being throughout their cancer journey.
Weighing Financial Implications and Accessibility
The cost of cancer treatment is an ethical consideration that pervades the healthcare landscape. The pursuit of effective treatments must be accompanied by a reflection on the financial burden placed on patients and society as a whole. Ensuring equitable access to treatments and exploring cost-effective alternatives are essential aspects of ethical decision-making in oncology. The goal is to strike a balance where financially sustainable treatment options are available without compromising patient well-being and the overall quality of care.
Ultimately, addressing the ethical considerations in cancer treatment calls for a delicate harmony between instilling hope, promoting quality of life, and acknowledging the real-world implications of cost. As the dreams for an effective cancer treatment in a brighter future persist, embracing these ethical values will guide the way towards a more compassionate and equitable oncology landscape.
From Bench to Bedside: Bridging the Gap in Translational Cancer Research
In the realm of oncology, the journey of discovering and developing new cancer treatments is a complex process that involves numerous stages and disciplines. While scientific innovations at the laboratory bench are crucial for advancements in cancer research, successful translation of these discoveries from the laboratory to clinical practice, commonly referred to as the "bedside," is equally critical. This article explores the challenges and significance of bridging the gap between laboratory investigation and patient care in the realm of translational cancer research.
Translational cancer research aims to bring the promising discoveries made in the laboratory to the real-world setting of clinical practice. It involves the seamless integration of basic science, preclinical studies, and clinical trials to ensure that novel treatments and interventions developed in laboratories are safe, effective, and accessible to cancer patients. This bridging process involves multidisciplinary collaborations, meticulous data collection, analysis, and interpretation, as well as rigorous evaluation through clinical trials. Success in translational research not only leads to improved cancer treatments but also contributes to the overall understanding of the disease.
- The Importance of Collaboration: Translational cancer research relies heavily on collaborations between scientists, clinicians, and other experts in various fields. This multidisciplinary approach ensures that diverse perspectives and expertise are brought together to overcome the challenges that arise during the translation process.
- Preclinical Studies: Before a new treatment or intervention can be tested on human subjects, it undergoes rigorous preclinical studies. These studies involve testing the treatment in animal models to evaluate its effectiveness, toxicity, and potential side effects. Preclinical studies provide valuable insights into the treatment's safety profile and help identify potential issues that need to be addressed before moving forward with clinical trials.
- Clinical Trials: Clinical trials are the final stage of translational cancer research, where the safety and effectiveness of new treatments are evaluated in human subjects. Through carefully designed protocols, clinical trials collect data on treatment outcomes, patient responses, and potential side effects. These trials serve as the gold standard for determining the success or failure of a new treatment and provide evidence for regulatory approval.
Successfully bridging the gap between bench and bedside requires efficient communication, extensive planning, and meticulous execution. It involves addressing technical, regulatory, logistical, and financial challenges to ensure that promising laboratory discoveries are translated into effective cancer treatments available to patients. The collaboration between researchers, clinicians, regulatory bodies, and funding agencies is crucial in driving forward the field of translational cancer research and ultimately improving patient outcomes.
FAQ
What is the article "Dreams of an Effective Cancer Treatment for a Brighter Future" about?
The article discusses the aspirations for an effective cancer treatment that would pave the way for a brighter future in the management of the disease.
What are some of the challenges in developing an effective cancer treatment?
Developing an effective cancer treatment faces various challenges, such as understanding the complex nature of cancer cells, anticipating potential side effects, and ensuring the treatment's accessibility and affordability.
What advancements have been made in cancer treatment research?
Advancements in cancer treatment research include the development of targeted therapies, immunotherapies, and precision medicine approaches, which have shown promising results in specific cancer types.
How important is early detection in the effective treatment of cancer?
Early detection plays a crucial role in the effective treatment of cancer as it increases the chances of successful intervention, improves treatment outcomes, and potentially reduces the need for aggressive therapies.
What are some hopes and dreams for the future of cancer treatment?
The future of cancer treatment holds hopes for personalized therapies, breakthrough discoveries, improved survivorship rates, and ultimately a world where cancer becomes a manageable chronic disease.
How common is cancer nowadays?
Cancer is becoming increasingly common, with statistics showing that one in three individuals will be diagnosed with some form of cancer in their lifetime.